Disease outbreaks are inherent to a populous, globalized world.
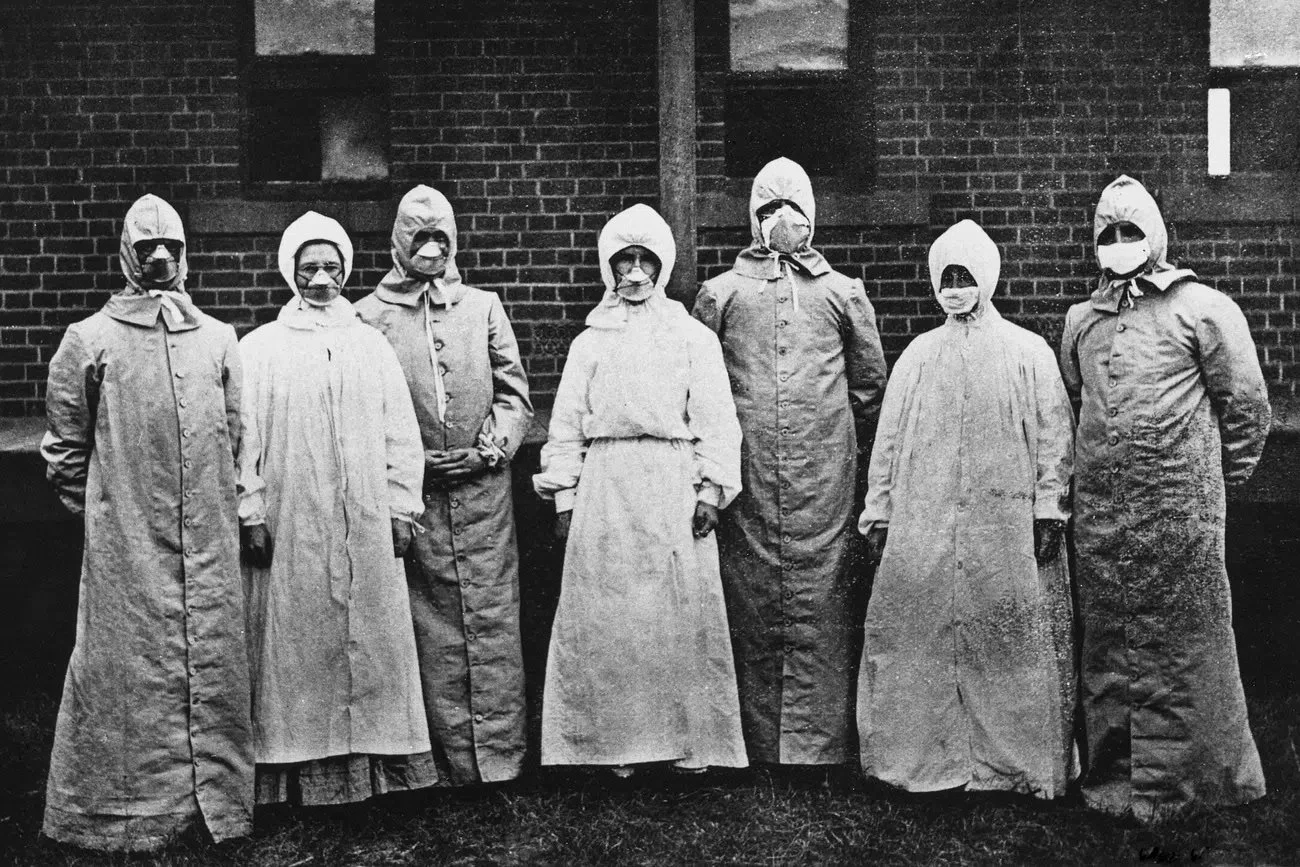
Doctors and nurses in biohazard suits during the 1918 Spanish Flu epidemic. National Museum of Health and Medicine. CC0.
Pandemics have been a part of the human story since the agricultural revolution in 10,000 BC. Agriculture gave people the ability to create more food than they ever had before, which meant that the human population soared. People began packing together and settling down in large communities without modern sanitation, creating the ideal conditions for the spread of disease. As time went on, larger and larger communities established extensive trading networks with the ability to spread disease across continents.
With each disease outbreak, humanity has developed better defenses and practices to help prevent catastrophic losses. However, as long as population sizes continue to rise and the global community becomes ever more interconnected, worldwide pandemics will always be something that humanity must contend with.
Sign up for our newsletter here!This trend towards an increasingly populous and interconnected world is what fueled the global sweep of the COVID-19 pandemic. As Amesh Adalja, MD, a senior scholar at Johns Hopkins Center for Health Security said, “Viruses used to spread at the speed of a steamboat. Now, they can spread at the speed of a jet. In that sense, we’re more at risk.” The only way to adapt to the expanding threat of disease is to learn from the past and prepare for the trends of the future. Below is a list of some of the most devastating pandemics in history and how humanity’s response to disease changed because of them.
1. The Bubonic Plague
14th Century CE
The plague of Florence, 1348. Boccacio’s Decam Wellcome. CC-BY-4.0.
Also known as the Black Death, the Bubonic Plague is the most notorious pandemic in history. It is believed to have killed between 30–50% of the European population in the 14th century, anywhere between 75 million and 200 million people. The Bubonic Plague is also thought to have killed 25 million people in Asia and Northern Africa at the time. The Black Death is known to have an incredibly high mortality rate, killing between 30-100% of those afflicted depending on the manner of infection.
Sign up for our newsletter here!The Bubonic Plague spread globally as a result of the Silk Road, which connected the world through trade networks. Rodents carrying fleas infected with the plague were easy stow-aways in trading caravans and vessels. This is one of the first instances where globalization caused a deadly, widespread disease outbreak.
At the time, the Black Death was thought to be the result of a combination of bad air, an imbalance in the body’s fluids or “humors,” and the wrath of God. Treatments included potions, fumigations, bloodletting, pastes, animal cures and religious cures. Persecution of minority groups was also common, particularly the Jewish population, who became a scapegoat for the suffering caused by the plague. Despite the outlandish and sometimes brutal practices of the 14th century, one method developed in the wake of the Black Death has proved incredibly effective: quarantine. Though, like today, many medieval citizens did not abide by quarantine practices, implementation of — to use a contemporary term — social distancing was one of the few effective practices to slow the spread of the Bubonic Plague.
2. Tuberculosis
7,000 BC – present day
A sick woman lies on a balcony with death standing over her, representing tuberculosis. Richard Tennant Cooper. CC-BY-4.0.
Sign up for our newsletter here!The sheer scope of tuberculosis in human history is almost difficult to fathom. Tuberculosis in humans can be traced back 9,000 years to Atlit Yam, a city now under the Mediterranean Sea, where archeologists found the disease in the bodies of a mother and child buried together. Tuberculosis, which has gone by many names throughout time, including “the white death” in the 1700s and “consumption” in the 1800s, is one of humanity’s great enemies. According to the CDC, from the 1600s–1800s, Tuberculosis was responsible for 25% of all deaths.
Today, vaccines and antibiotics are available to prevent and treat tuberculosis. These developments in tuberculosis treatments saved 74 million lives between 2000 and 2021. However, despite this breakthrough in modern medicine, a total of 1.6 million people died from tuberculosis in 2021 according to the World Health Organization. Over 80% of these deaths come from low and middle income countries. Modern medicine means that Tuberculosis is treatable, but these treatments are not universally accessible. In a globalized world, access to healthcare cannot be a first world luxury if outbreaks are to be prevented.
3. The Columbian Exchange
1492–1800 CE
Spanish imperialists conquer the Americas. Wilfredor. CC-BY-SA.
Sign up for our newsletter here!The Columbian Exchange is a massive interchange of people, animals, plants, and diseases that took place between Eastern and Western Hemispheres after Columbus’ arrival in the Americas in 1492. This process introduced a number of foreign diseases that Native Americans had no immunity to, whose toll reached genocidal proportions, killing between 80–95% of Indigenous Americans within 100–150 years of Columbus’ first landing. Some of the diseases that plagued the Native Americans include smallpox, measles, influenza, chickenpox, the bubonic plague, typhus, scarlet fever, pneumonia and malaria. European imperialism is to blame for the catastrophic spread of disease to the Indigenous population.
4. The Spanish Flu
1918–1919 CE
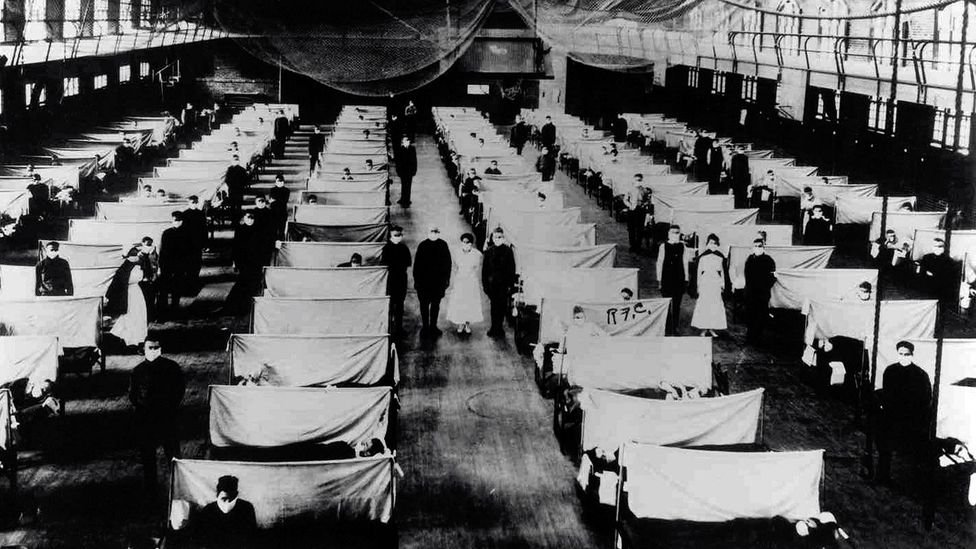
Infected patients were isolated during the 1918 Spanish Flu pandemic. Jim Forest. CC-BY-NC-ND 2.0.
After WWI, global contact and poor sanitary conditions during the war caused a worldwide outbreak of the H1N1 influenza virus, known at the time as the Spanish Flu. 500 million people were infected, one third of the world’s population at the time. Of those infected, 50 million people died worldwide, including 675,000 people in the United States.
Sign up for our newsletter here!This pandemic led to a number of medical innovations still in use today. One of which is the widespread use of masks to prevent the spread of disease. The Spanish Flu pandemic also led to innovations in vaccine technology and spurred our understanding of genes and the chemicals that encode them.
5. AIDS Epidemic
1981-1990s
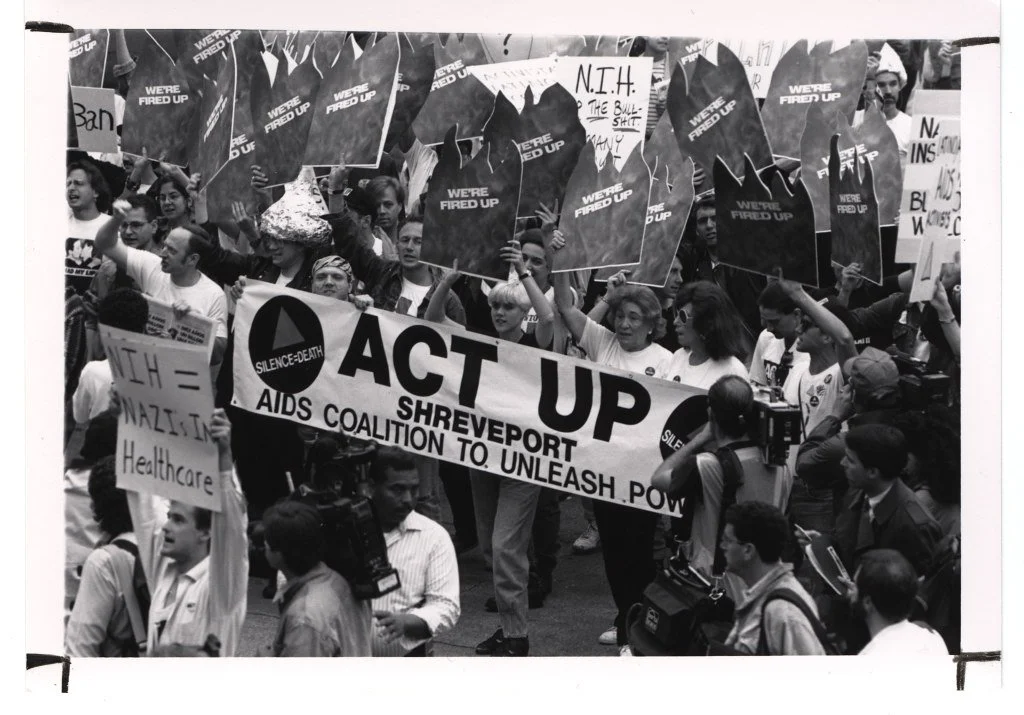
Protestors march against the stigma caused by the AIDs epidemic. NIH History Office. CC0.
HIV originally jumped from chimpanzees to humans in the early ‘80s, most likely due to human hunters coming into contact with chimpanzee blood. As a result, 84 million people have been infected globally and 40 million people have died. The AIDS epidemic is notorious for the resulting stigmatization of the LGBTQ+ community, which were greatly, though not uniquely, affected by the disease. Epidemics throughout history, since the Bubonic Plague, have caused hysteria and scapegoating, a flaw in human nature that must be quelled.
Sign up for our newsletter here!Since the 1980s incredible strides have been made in the treatment of HIV and AIDS. As of 2021, 38.4 million people were living with HIV without it progressing to AIDS (when deadly symptoms appear) due to modern treatments. The treatment for HIV is taking daily antiretroviral therapy (ART), which is a cocktail of different HIV medicines. This treatment can allow people to live with HIV for decades without it progressing to AIDS.
Sophia Larson
Sophia Larson is a recent graduate of Barnard College at Columbia University. She previously worked as the Assistant Editor on the 2021 book Young People of the Pandemic. She has also participated as a writer and editor at several student news publications, including “The UMass Daily Collegian” and “Bwog, Columbia Student News.”